What is insomnia, and how is it treated?
Do you think you might have insomnia?
- Do you have difficulty falling or staying asleep?
- Are you worried about your sleep?
- Does your sleep impact your mood, relationships, or work during the day?
If your answer to any of these questions was yes, you may be experiencing insomnia.

What is insomnia?
 Insomnia is a chronic difficulty with getting to sleep or staying asleep. This has a negative impact on wellbeing and can cause a great deal of distress. At sleep Matters, we help adults, children and adolescents with insomnia and other forms of disturbed sleep.
Insomnia is a chronic difficulty with getting to sleep or staying asleep. This has a negative impact on wellbeing and can cause a great deal of distress. At sleep Matters, we help adults, children and adolescents with insomnia and other forms of disturbed sleep.
Insomnia is one of the most common complaints people discuss with their GP. Australian research suggests that 1 in 3 people have difficulty sleeping. 1 in 10 Australians meet the criteria for a diagnosis of insomnia Disorder.
Insomnia Disorder is not just an occasional night of poor sleep. Rather, it’s a chronic sleep problem that has a large impact on wellbeing and often continues long after the initial cause of the poor sleep has disappeared. It can take the form of chronic difficulty falling asleep (sleep onset insomnia) and/or returning to sleep (sleep maintenance insomnia) following night-time awakening. The insomnia can feel out of control, like it has a life of its own. The harder the poor sleeper tries to sleep, the more awake they become.
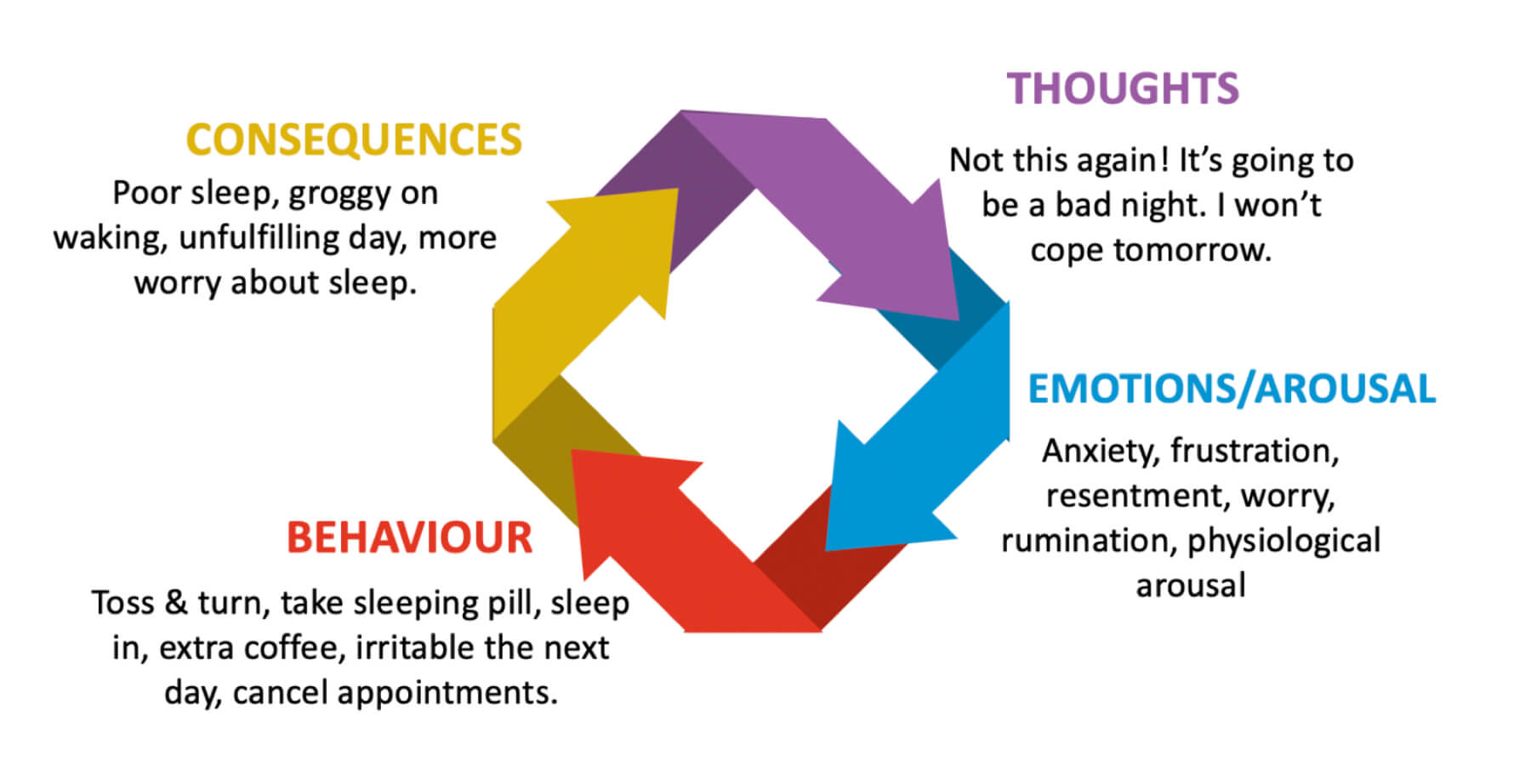
Once insomnia takes hold and becomes chronic, the situation can cause unhelpful sleep habits and high levels of anxiety and worry. These habits and worries keep the problem going.
Insomnia reduces quality of life, and can increase the likelihood of developing additional problems such as depressed mood and anxiety.
What causes insomnia?
The initial cause of insomnia is not always the same as what maintains it (keeps it going).
What makes someone more prone to insomnia?
Genetics - biologists have found a genetic link. Thankfully, a genetic predisposition doesn’t make it untreatable.
Stress - heavy workload, relationship problems, life changes
Stress-reactivity - people who respond strongly to stress are prone to sleep disturbance
People who identify as ‘worriers’
Depression
Anxiety disorders
Menopause Insomnia
Pregnancy Insomnia
Advancing age
Medical conditions such as reflux (GORD), hyperthyroidism, chronic pain, other sleep disorders, ADHD, nasal/sinus conditions
Certain medications
Poor sleep environment: e.g., noisy, light, uncomfortable
Irregular sleep routine
What keeps insomnia going?
Unhelpful sleep habits - irregular sleep schedule, long naps, spending too long in bed, not winding down before bed, alcohol before bed, reliance on sleeping pills.
Changing daytime routines - withdrawing from usual activities such as the gym, work, or socialising.
Mental busyness - overthinking and general worry, as well as worry and preoccupation with sleep and tiredness.
Concern about sleep can lead to coping behaviours which backfire. For example, going to bed early, sleeping in, and napping can make solid sleep harder to achieve. Drinking excess coffee, not going to the gym and withdrawing from life due to fatigue can also worsen sleep and increase worry about it.
A vicious cycle can develop where poor sleep leads to worry and unhelpful habits which leads to worse sleep.
How is insomnia diagnosed?
Insomnia Disorder is usually straightforward to diagnose on the basis of a clinical interview, a sleep log, and brief screening questionnaires. The diagnosis is based on your report of symptoms, not on a biological test or an overnight sleep study. We may, however, suggest that we assess your sleep overnight so that we can screen for other sleep disorders and have an objective view of your sleep quality and timing.
At Sleep Matters Perth we will ask you to complete a sleep log for a week prior to your initial appointment, along with some brief screening questionnaires about your sleep.
Do I have insomnia? Take our quiz.
Take our short quiz to see if your symptoms are key indicators.Insomnia treatments
The good news is that insomnia is a condition that usually responds well to treatment. Sometimes clients need as few as 4-6 consultations to get back to better sleep. The clincial team at Sleep Matters are trained in CBT-Insomnia, the recommended first-line treatment.
There are a number of diverse cures and treatments, some more effective than others. The recommended first-line treatment is Cognitive Behaviour Therapy-Insomnia, or CBT-I.
Evidence-based treatments used at Sleep Matters:
Cognitive Behaviour Therapy for Insomnia (CBT-I)
Mindfulness-based approaches
Light therapy
Stress management
Melatonin
Sleeping pills (recommended for short term use only)
Over the counter remedies
Cognitive Behaviour Therapy for Insomnia (CBT-I)
At Sleep Matters, we specialise in Cognitive Behavioural Therapy for Insomnia (CBT-I). Approximately 70-80% of people with insomnia obtain lasting benefit from this treatment. Research shows that it is more effective than sleeping pills in the long term. CBT-I isn’t a quick fix, but a longstanding approach to managing insomnia by addressing what keeps the problem going. It is important that your treating clinician has specific training and experience with helping people to identify and change unhelpful thoughts, beliefs, and behaviours.
Mindfulness and Acceptance-Based approaches to Insomnia
Mindfulness can be a stand-alone treatment or combined with other approaches, such as CBT and Acceptance and Commitment Therapy. The main thrust of ACT is to help you create a rich and meaningful life. Mindfulness teaches you to accept difficult thoughts and feelings rather than struggling with them. This frees you up to do the things that really matter in life.
Stress Management and Insomnia
Sleep hygiene
Sleep Hygiene is a term that describes how to set up a healthy sleep routine. You could find a list of recommendations for good sleep with a quick search of the internet. Clinical trials tell us that there is more to treatment than just following a list of sleep tips, even though they may be a helpful part of the solution.
Our infographic on sleep hygiene contains important tips for improving sleep and setting up a healthy sleep routine. This isn't an exhaustive list, but is a carefully considered selection of changes that can have a large impact.
Hypnosis
Melatonin
Sleeping pills
Did you know that sleeping tablets are usually meant for short-term use? Most sleeping pills are not meant to be taken for more than about 3-4 weeks.
Australian research suggests that about 95% of people who consult their GP with Insomnia are prescribed sleeping pills. However, peak professional bodies recommend Cognitive Behaviour Therapy CBT-I as the first line treatment.
At Sleep Matters we often assist people to reduce or eliminate their use of sleeping pills, allowing them to become confident about their ability to sleep naturally.
Over the counter remedies
Many individuals with insomnia don’t seek professional help, but rather use self-help remedies. Common over-the-counter remedies include antihistamines (eg. restavit, phenergan), valerian, hops, kava, passion flower, tart cherry juice, lavender, and chamomile.
Unfortunately, the research on the effectiveness of herbal remedies and over the counter preparations for insomnia isn’t yet thorough enough. This means that these treatments don’t have enough evidence to be a recommended treatment.
I think I have insomnia, what should I do next?
If you think you have insomnia, it’s a good idea to see your GP as they will be able to screen you for any underlying conditions. Your GP can refer you to Sleep Matters. If you are referred under a mental health care plan, you can receive Medicare rebates that reduce your out-of-pocket expense.
You are also welcome to attend sleep Matters without a referral, in which case you can use private health rebates.
Our experience matches what clinical research trials tell us. Insomnia can usually be treated even when it is long term, and when there are other conditions present.
Be sure to check out our blog for lots of information about all matters sleep.