Pri Mithal, BSc. (Hons), MPsych (Clin)
Clinical Psychologist Registrar
“Sleep is the golden chain that ties health and our bodies together.” — Thomas Dekker

Ahh…sleep…zzzzz. Some of us love it, and others dread it.
Here we debunk a few sleep myths, consider what healthy sleep is and when to seek help for trouble sleeping.
So, what exactly is sleep and why do we need it? Sleep is often thought of as a state of rest. Through medical technology scientists have been able to study the brain whilst a person is asleep. What they have found is that sleep is actually quite an active process and during this time, our brain and body go through various important actions to boost our health and overall functioning. Whilst sleeping, our brain plays a “housekeeping” role, whereby memories are processed, toxins are removed, learning is consolidated, and parts of our body are restored and repaired.
What is “healthy” sleep?
There is often confusion around what “normal” sleep entails, and people can find themselves getting worked up about common fluctuations and disruptions in sleep patterns. Here are a couple notable facts about sleep that might help you rest easier.
How we sleep has drastically changed from how our ancestors used to sleep. In ancient times, people slept in two shifts, with 1-3 hours break in the middle to engage in various activities, such as praying, visiting neighbours, eating, drinking, having quiet time, or simply completing a task. Dreams were thought to be a way of receiving messages from the gods, with people sleeping in temples or caves to get answers to questions about their lives. In modern society, sleep has shifted to longer bouts of sleep overnight to suit busy 9-5 schedules that enable us to work and contribute to society.
In the age of social media, we are constantly bombarded with mixed messages around sleep. There has been a recent emergence in productivity enthusiasts who put forth messages like “Sleep is for the weak.” or “You can sleep when you’re dead.” Needing less sleep and bragging about it, has become a new cultural norm, especially in Western society, where work and goal-based pursuits are valued more over rest and relaxation. However, we know from research that sleeping any less than 5.5 hours can be detrimental to our long-term health and well-being. However, if you do know someone who can sleep less than 5.5 hours and function fine, it could be due to a rare genetic mutation. Nevertheless, the bottom line is that we cannot “train” our bodies to sleep less.
On the other end of the spectrum, we hear messages like “You must get a minimum of 8 hours of sleep to function.” or that “insomnia can be lethal.” Again, research has debunked these myths. In actuality, “normal” sleep varies from person to person. Even though the average normal amount of sleep is 6-8 hours per night, some people naturally can sleep lesser (around 5 hours; *see above), and some need more sleep (9-10 hours) to function. Just like shoe size or height, what is considered normal sleep for you can be different for someone else.
The main idea here is that your body decides how much sleep it needs. Much like digestion and breathing, sleep is a biological process that is usually well regulated by the brain, but we can complicate sleep by trying to take over and micromanage it. No one likes a micromanager, and that includes your sleep! Indeed, a new term has been coined recently to refer to the condition where people are obsessive and perfectionistic about their sleep: orthosomnia . Orthosomnia is associated with poorer sleep health and is a nice reminder that while we should be sensible in our approach to sleep, that it’s not helpful to overthink it.
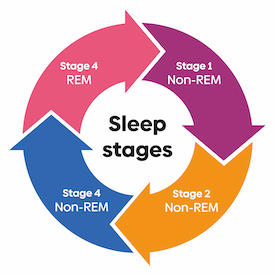
Sleep occurs in stages. Most people think that sleep should happen as soon as our head hits the pillow, and continue into deep sleep, until we awaken in the morning feeling fresh and rejuvenated. However, this is not actually the case.
Sleep occurs in 90-minute cycles overnight, with frequent awakenings being quite common. In general, there are five sleep stages that we go through, and after 90-minutes, we awaken (sometimes very briefly), until we settle back into the next sleep cycle. These 5 stages include a drowsiness, light sleep, moderate sleep, deep sleep and REM sleep. To read more about sleep stages please see: https://www.sleepfoundation.org/stages-of-sleep. The bottom line here is that it is normal to wake up in the middle of the night. In fact, your body needs this to progress into the next stage of sleep. Some people can drift through this “awakening” and have little memory of this time. However, others can be a bit more sensitive to arousal and can find themselves wide awake. If this is you, it is important to note that finding yourself awake in the middle of the night is normal. However, fixating on this and making mental calculations around how much sleep you have left, can activate your brain and this is when you might find yourself tossing and turning.
Is it time for me to see a health professional such as a psychologist for trouble sleeping?
1 in 3 Australians report regular poor sleep. However, around 10% of these suffer from what is known as Insomnia Disorder (aka chronic insomnia). Experiencing chronic insomnia is different from the very typical sleep disruptions described above. Insomnia a longstanding issue where sleep is disrupted at least 3 nights a week for at least 3 months. To gauge whether you might be experiencing insomnia, look for the following signs over a long-term period:
- Difficulty falling asleep
- Difficulty staying asleep characterized by trouble going back to sleep once awakened
- Early- morning awakenings with an inability to return to sleep
- Significant distress or impairment in daytime functioning
Insomnia can be linked to psychological issues such as stress, anxiety, or depression. When we experience psychological distress, we may have negative thoughts, worries, and low mood, that could impact our sleep. For instance, many people with insomnia report staying up late into the night thinking about memories of the past or the future. Others get tangled into negative thoughts about their sleep or worries about the next day. Some people are chronically stressed, with their brain producing stress hormones such as cortisol and adrenaline that keep them in a “fight or fight” state, which is counteractive to rest and relaxation. Often, people continue to sleep poorly even after the stress has resolved. For example, a new parent may experience disrupted sleep whilst baby wakes overnight, only to find that they still have trouble sleeping even when the baby is slumbering through. It’s as if the poor sleep has become a habit and has taken on a life of its own.
If you find yourself having such difficulties, it could mean that you require an evidence-based intervention for your sleep difficulties. A psychologist with training in behavioural sleep medicine can provide Cognitive Behavioural Therapy for insomnia (CBT-I), which is the gold-standard treatment for longstanding sleep problems described above.
The cognitive (“thinking”) component of CBT-I helps people develop more helpful thoughts and attitudes about sleeping. The behavioural component helps people alter habits that get in the way of sleeping well. Research on CBT for insomnia has found that it not only addresses the factors maintaining long-term insomnia, but it also leads to more long-lasting improvements than sleep medications. In Australia, and many other countries, CBT-I is the recommended first-line treatment for insomnia. At Sleep Matters, our psychologists are trained in an utilise CBT for insomnia chronic insomnia. This can be done through individual therapy sessions (approximately 5-8 sessions). We also offer a group therapy program that can be attended over the course of 4 sessions (2 hours each). To inquire further, please call our clinic at: 6107 6828. Please note that a Mental Health Care Plan can be obtained through a GP referral which allows access to Medicare rebates. For those not accessing Medicare rebates, private health rebates may apply.
We’d love to help you on the path to sleeping better. To find out more about our sleep treatment programs, please see: https://www.sleepmattersperth.com.au/sleep-psychologist-perth/
Blog overview